Proteksi Radiasi Pada Terapi Radionuklida
Keywords:
radiasi pengion, pelayanan kesehatan, proteksi radiasi, terapi radionuklidaSynopsis
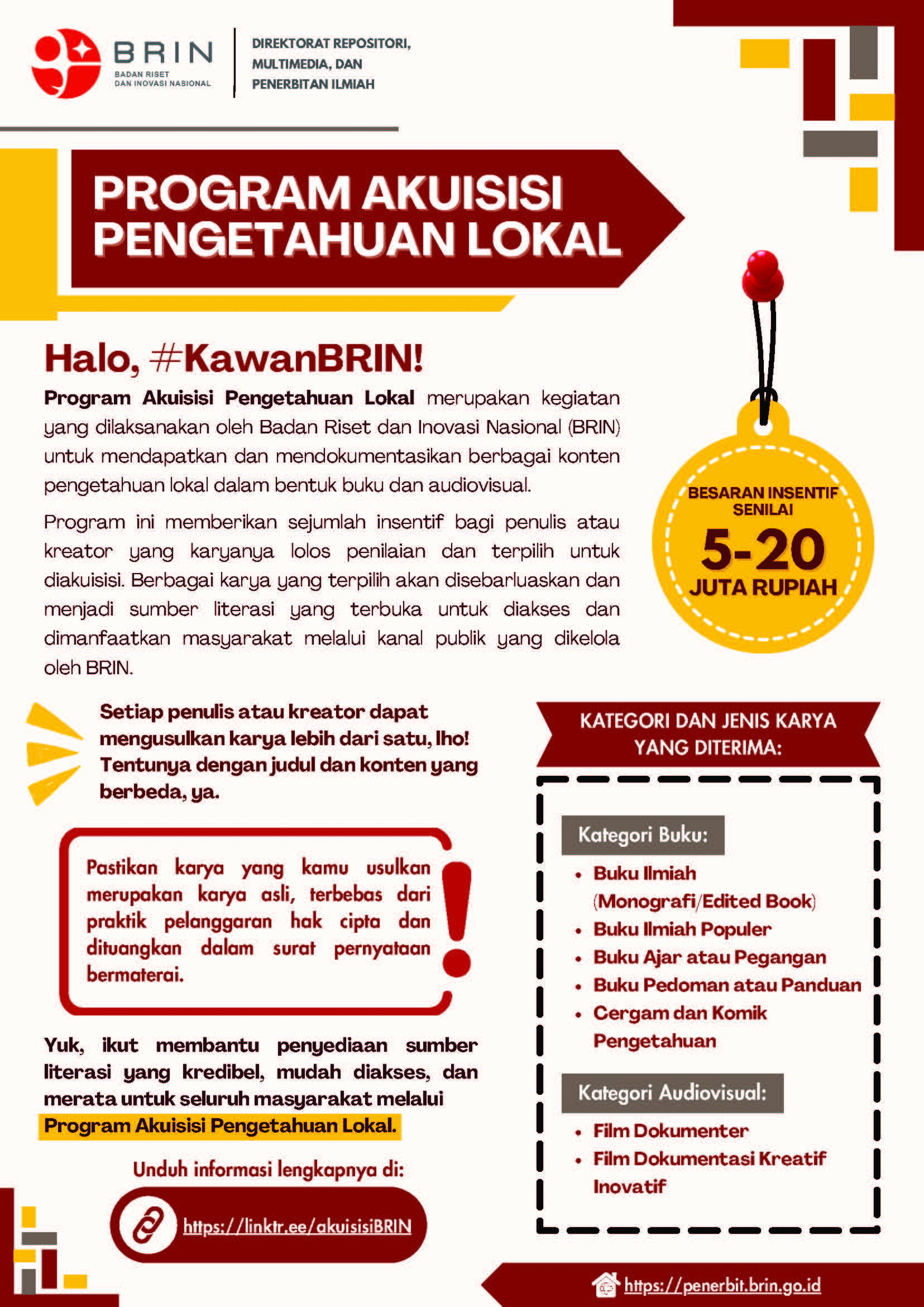
Terapi radionuklida merupakan salah satu pemanfaatan sumber radiasi, yang juga disebut sebagai radionuklida, di bidang medis. Sumber radionuklida tersebut diikat kuat dengan suatu molekul biologi, atau farmaka, sehingga disebut sebagai radiofarmaka. Keuntungan terapi radionuklida adalah mampu memberikan dosis serap yang sangat terkonsentrasi pada tumor target dan tidak memberikan dosis ke jaringan sehat di sekitarnya. Sumber radionuklida yang digunakan umumnya merupakan pemancar beta atau alfa, dan sedikit pemancar gamma. Aktivitas radiasi yang digunakan juga cukup rendah.
Namun demikian, sebgai sumber radiasi, radiofarmaka juga memiliki potensi bahaya yang perlu dikelola dengan baik. Buku ini menguraikan pokok-pokok tindakan proteksi radiasi yang perlu dilakukan agar tindakan terapi radionuklida dapat berjalan dengan aman dan selamat. Tindakan proteksi radiasi yang perlu dilakukan adalah sejak pasien dipersiapkan di rumah sakit untuk menerima radiofarmaka hingga pasien pulang ke rumah. Bahkan, tindakan proteksi radiasi perlu juga dilakukan jika pasien meninggal dalam perawatan dan kemudian akan dimakamkan atau dikremasi, dan juga dibalsem untuk pengawetan jika akan dikirim dari satu lokasi ke lokasi lain dalam waktu yang agak lama.
Buku ini diharapkan dapat menjadi pedoman untuk berbagai pihak yang terlibat dalam tindakan terapi radionuklida, mulai dari para tenaga medis, fisikawan medis, perawat, hingga petugas proteksi radiasi, dan juga pendamping pasien, dalam mengambil tindakan yang tepat dari sisi proteksi dan keselamatan radiasi.
Downloads
References
Administration of Radioactive Substances Advisory Committee-Health Security Agency (ARSAC-HAS). (2024). Notes for guidance on the clinical administration of radiopharmaceuticals and use of sealed radioactive sources. https://assets.publishing.service.gov.uk/media/65f997f9703c42001158ef75/Notes-for-guidance-on-the-clinical-administration-of-radiopharmaceuticals-and-use-of-sealed-radioactive-sources.pdf
Asadian, S., Mirzaei, H., Kalantari, B. A., Davarpanah, M. R., Mohamadi, M., Shpichka, A., Nasehi, L., Es, H. A., Timashev, P., Najimi, M., Gheibi, N., Hassan, M. & Vosough, M. (2020). B-radiating radionuclides in cancer treatment, novel insight into promising approach. Pharmacol. Res., 160, 105070. https://doi.org/10.1016/j.phrs.2020.105070
Assadi, M., Gholamrezanezhad, A., Jokar, N., Keshavarz, M., Picchio, M., Seregni, E., Bombardieri, E. & Chiti, A. (2020). Key elements of preparedness for pandemic coronavirus disease 2019 (COVID-19) in nuclear medicine units. European Journal of Nuclear Medicine and Molecular Imaging, 47, 1779–1786. https://doi.org/10.1007/s00259-020-04780-4
Australian Radiation Protection and Nuclear Safety Agency. (2002). Discharge of patients undergoing treatment with radioactive substances. https://www.arpansa.gov.au/regulation-and-licensing/regulatory-publications/radiation-protection-series/guides-and-recommendations/rps4
Australian Radiation Protection and Nuclear Safety Agency. (2008). Radiation protection in nuclear medicine. https://www.arpansa.gov.au/regulation-and-licensing/regulatory-publications/radiation-protection-series/guides-and-recommendations/rps14-2
Badan Pengawas Tenaga Nuklir. (2020). Ringkasan eksekutif pedoman teknis rilis pasien (release of patient) pada kedokteran nuklir.
https://cloud.bapeten.go.id/index.php/s/5tMApat96nFwj6W#pdfviewer
Barrington, S. F., Kettle, A. G., O’Doherty, M. J., Wells, C. P., Somer, E. J. & Coakley, A. J. (1999). Radiation dose rates from patients receiving iodine-131 therapy for carcinoma of the thyroid, 23(2), 123–130. https://doi.org/10.1007/BF01731834
Bly, R. (2020). Radiation protection issues in radionuclide therapy – workers (medical staff), third persons, waste management. Dalam EU Scientific Seminar November: Developments in nuclear medicine–new radioisotopes in use and associated challenges, Proceedings of a scientific seminar held in Luxembourg on 13 November 2019, Radiation Protection No. 194. European Commission.
WT.mc_id=Searchresult&WT.ria_c=37085&WT.ria_f=3608&WT.ria_ev=search
Budiawan, H. (2018). Nuclear theranostics in Indonesia: Past, present, and future. Nuclear Medicine and Molecular Imaging, 53, 33–34. https://doi.org/10.1007/s13139-018-0561-6
Burkett, B. J., Dundar, A., Young, J. R., Packard, A. T., Johnson, G. B., Halfdanarson, T. R., Eiring, R. A., Gansen, D. N., Patton, C. M. & Kendi, A. T. (2021). How we do it: A multidisciplinary approach to 177Lu DOTATAE peptide receptor radionuclide therapy. Radiology, 298, 261–262. https://doi.org/10.1148/radiol.2020201745
Cember, H. & Johnson, T. E. (2009). Introduction to health physics (4th ed., 73). McGraw Hill Medical.
Dauer, L. T. (2014). Management of therapy patients. Dalam D. L. Bailey, J. L. Humm, A. Todd-Pokropek, & A. van Aswegen (Ed.), Nuclear medicine physics: A handbook for teachers and students. IAEA.
https://www.iaea.org/publications/10368/nuclear-medicine-physics
Ersahin, D., Doddamane, I. & Cheng, D. (2011). Targeted radionuclide therapy. Cancers, 3, 3838–3855. https://doi.org/10.3390/cancers3043838
Escopharma (t.t.). Radiopharmacy compounding equipment. Diakses 21 Maret 2024, dari https://www.escopharma.com/pdf/brochures/Radiopharmacy-Compounding-Equipment-vA-A4-LR.pdf
Evani, S. (t.t.). Penggunaan alat pelindung diri untuk mencegah penyakit infeksius pada tenaga medis dalam menghadapi pandemi Covid-19. Diakses 23 Juli 2024, dari https://www.alomedika.com/penggunaan-alat-perlindungan-diri-untuk-mencegah-penyakit-infeksius-pada-tenaga-medis
Garcia-Baonza, R., Sáez-Muñoz, M., Candela-Juan, C., Rozas, S., Camp, A., Martinez & Andresz, A. (2022). COVID-19 pandemic impact on the Spanih radiation protection professionals. Radioprotection, 57(3), 233–240
https://doi.org/10.1051/radiopro/2022016
Goldsmith, S. J. (2020). Targeted radionuclide therapy: A historical and personal review. Seminars in Nuclear Medicine, 50(1), 87–97. https://doi.org/10.1053/j.semnuclmed.2019.07.006
Hidayati, N. R., Setyowati, S., Sutari, Triningsih, Karyadi, Aguswarini, S., Humani, T. S., Hidayat, B., Ramli, M., Massora, S., Susilo, V. Y., Mutalib, A., Sastramihardja, H. & Masjhur, J. S. (2015). Studi awal estimasi dosis internal 177Lu-DOTA Trastuzumab pada manusia berbasis uji biodistribusi pada mencit. Jurnal Sains dan Teknologi Nuklir Indonesia, 16(2), 105–116.
https://dx.doi.org/10.17146/jstni.2015.16.2.2362
Hidayati, N. R., Poon, A., Willowson, K., Eslick, E., Ryu, H. & Bailey, D. L. (2019). Evaluation of kidney dose in neuroendocrine tumors patients after peptide receptor radionuclide therapy using 177Lu-DOTATATE. Atom Indonesia, 45(3), 147–152.
https://doi.org/10.17146/aij.2019.910
Hiswara, E. (2023). Istilah dan definisi dalam proteksi dan keselamatan radiasi. Penerbit BRIN. https://doi.org/10.55981/brin.522
Hoefnagel, C. A., den Hartog Jager, F. C. A., Taal, B.G., Abeling, N. G. G. M. & Engelsman, E. E. (1987). The role of I-131-MIBG in the diagnosis and therapy of carcinoids. European Journal of Nuclear Medicine, 13, 187–191. https://doi.org/10.1007/BF00256489
Humas BRIN. (2023, 8 Desember). Tantangan nuklir bidang kesehatan, PKN-TMI: fasilitas kedokteran nuklir dan radiofarmaka terbatas. BRIN. https://www.brin.go.id/news/117035/tantangan-nuklir-bidang-kesehatan-pkn-tmi-fasilitas-kedokteran-nuklir-dan-radiofarmaka-terbatas
Humas Unand. (2023, 8 Maret). Guru besar FK UNAND kenalkan kedokteran nuklir yang masih asing di Indonesia. Universitas Andalas. https://www.unand.ac.id/index.php/berita/9-seputar-unand/379-gubes-fk-unand-kedokteran-nuklir.html
Idee, J-M., Louguet, S., Ballet, S. & Corot, C. (2013). Theranostics and contrast-agents for medical imaging: a pharmaceutical company viepoint. Quantitative Imaging in Medicine and Surgery, 3(6), 292–297. https://doi.org/10.3978/j.issn.2223-4292.2013.12.06
International Atomic Energy Agency. (t.t.-a). Radiation protection in nuclear medicine. Diakses 20 Maret 2024, dari https://www.iaea.org/resources/rpop/health-professionals/nuclear-medicine
International Atomic Energy Agency. (t.t.-b). Radionuclide therapy. Diakses 7 Februari 2024, dari https://www.iaea.org/topics/radionuclide-therapy
International Atomic Energy Agency. (t.t.-c). Specific therapies involving radiation. Diakses 7 Februari 2024, dari https://www.iaea.org/resources/rpop/health-professionals/nuclear-medicine/therapeutic-nuclear-medicine/specific-therapies
International Atomic Energy Agency. (1996a). Manual on therapeutic uses of iodine-131. https://www.iaea.org/publications/4596/manual-on-therapeutic-uses-of-iodine-131
International Atomic Energy Agency. (1996b). International basic safety standards for protection against ionizing radiation and for the safety of radiation sources. https://gnssn.iaea.org/Superseded%20Safety%20Standards/Safety_Series_115_1996_Pub996_EN.pdf
International Atomic Energy Agency. (2007). Arrangements for preparedness for a nuclear or radiological emergency. https://www.iaea.org/publications/7503/arrangements-for-preparedness-for-a-nuclear-or-radiological-emergency
International Atomic Energy Agency. (2011). Criteria for use in preparedness and response for nuclear or radiological emergency. https://www.iaea.org/publications/8506/criteria-for-use-in-preparedness-and-response-for-a-nuclear-or-radiological-emergency
International Atomic Energy Agency. (2009a). Release of patients after radionuclide therapy. https://www.iaea.org/publications/8179/release-of-patients-after-radionuclide-therapy
International Atomic Energy Agency. (2009b). Classification of radioactive waste. https://www.iaea.org/publications/8154/classification-of-radioactive-waste
International Atomic Energy Agency. (2009c). Predisposal management of radioactive waste. https://www.iaea.org/publications/8004/predisposal-management-of-radioactive-waste
International Atomic Energy Agency. (2011). Disposal of radioactive waste.
https://www.iaea.org/publications/8420/disposal-of-radioactive-waste
International Atomic Energy Agency. (2014a). Radiation protection and safety of radiation sources: International basic safety standards. https://www.iaea.org/publications/8930/radiation-protection-and-safety-of-radiation-sources-international-basic-safety-standards
International Atomic Energy Agency. (2014b). Modular design of processing and storage facilities for small volumes of low and intermediate level radioactive waste including disused sealed sources. https://www.iaea.org/publications/10484/modular-design-of-processing-and-storage-facilities-for-small-volumes-of-low-and-intermediate-level-radioactive-waste-including-disused-sealed-sources
International Atomic Energy Agency. (2015). Preparedness and response for a nulcear or radiological emergency. https://www.iaea.org/publications/10905/preparedness-and-response-for-a-nuclear-or-radiological-emergency
International Atomic Energy Agency. (2016) Storage of radioactive waste.
https://www.iaea.org/publications/7441/storage-of-radioactive-waste
International Atomic Energy Agency. (2018a). Radiation protection and safety in medical uses of ionizing radiation. https://www.iaea.org/publications/11102/radiation-protection-and-safety-in-medical-uses-of-ionizing-radiation
International Atomic Energy Agency. (2018b). Regulations for the safe transport of radioactive material https://www.iaea.org/publications/12288/regulations-for-the-safe-transport-of-radioactive-material
International Atomic Energy Agency. (2019). Predisposal management of radioactive waste from the use of radioactive material in medicine, industry, agriculture, research and education. https://www.iaea.org/publications/11087/predisposal-management-of-radioactive-waste-from-the-use-of-radioactive-material-in-medicine-industry-agriculture-research-and-education
International Atomic Energy Agency. (2020). Covid-19 pandemic: Technical guidance for nuclear medicine departments. https://www.iaea.org/publications/14733/covid-19-pandemic-technical-guidance-for-nuclear-medicine-departments
International Atomic Energy Agency. (2021). Quanum 3.0: An updated tool for nuclear medicine audits (3rd ed).
https://www.iaea.org/publications/13619/quanum-30-an-updated-tool-for-nuclear-medicine-audits
International Commission on Radiological Protection. (2004). Release of patients after therapy with unsealed radionuclides. ICRP Publication 94. Ann. ICRP, 34(2). https://icrp.org/publication.asp?id=ICRP%20Publication%2094
International Commission on Radiological Protection. (2012). Compendium of dose coefficients based on ICRP Publication 60. ICRP Publication 119. Ann. ICRP, 41(Suppl.) https://icrp.org/publication.asp?id=ICRP%20Publication%20119
Kartamihardja, A. H. S. (2013). Perkembangan kedokteran nuklir dan radiofarmaka di Indonesia. http://pustaka.unpad.ac.id/wp-content/uploads/2015/06/Perkembangan-KN-dan-RF-di-Indonesia.pdf
Kheruka, S. C., Shankar, N., Ora, M. & Ghambir, S. (2021). Do current radiation safety guidelines allow the safe release of a thyroid cancer patient after high-dose radioiodine therapy? An Indian perspective. Indian Journal of Nuclear Medicine, 36, 148-52. https://doi.org/10.4103/ijnm.ijnm_210_20
Kim, K. & Kim, S-J. (2018). Lu-177-based peptide receptor radionuclide therapy for advanced neuroendocrine tumors. Nuclear Medicine and Molecular Imaging, 52, 208–215. https://doi.org/10.1007/s13139-017-0505-6
Klaassen, N. J., Arntz, M. J., Arranja, A. G., Roosen, J. & Nijsen, J. F. W. (2019). The various therapeutic applications of the medical isotope holmium-166: A narrative review. EJNMMI Radiopharmacy and Chemistry, 4(19). https://doi.org/10.1186/s41181-019-0066-3
Lassen, S. A., Andersen, T. H., Liukonen, J., Pétursdóttir, N., Andersen, A. & Idestrom, L. (2023). Considerations for the release of patients after radionuclide therapy.
https://www.stralsakerhetsmyndigheten.se/en/publications/reports/nordic-series/022023/
Laurus Systems Inc. (t.t.). Ring dosimeters. Diakses 22 Maret 2024 dari https://www.laurussystems.com/wp-content/uploads/LS-Ring-Dosimetry.pdf
Lepareur, N., Lacœuille, F., Bouvry, C., Hindré, F., Garcion, E., Chérel, M., Noiret, N., Garin, E. & Knapp Jr., F. F. R. (2019). Rhenium-188 labeled radiopharmaceuticals: Current clinical applications in oncology and promising perspectives. Frontiers in Medicine, 6(132). https://doi.org/10.3389/fmed.2019.00132
Lubis, L. E., Nastiti, Y., Anam, C., Lestariningsih, I., Gani, M. R. A., Laksono, M. B., Fahmi, A. & Simanjuntak, J. (2020). Penggunaan radiasi pengion dalam diagnosis dan penanganan COVID-19. https://www.afismi.org/_files/ugd/b982fa_ea39ed9b5ce14f8c9aa040596ad7be21.pdf
Manumoyoso, A. H. (2023, 25 Agustus). Spesialis kedokteran nuklir perlu ditambah. Kompas. https://www.kompas.id/baca/humaniora/2023/08/25/spesialis-kedokteran-nuklir-perlu-ditambah
Menon, S. R., Mitra, A., Chakraborty, A., Tawate, M., Sahu, S., Rakshit, S., Gaikwad, S., Dhotre, G., Damle, A., & Banerjee, S. (2022). Clinical dose preparation of [177Lu] Lu-DOTA-Pertuzumab using medium specific activity [177Lu] LuCl3 for radioimmunotherapy of breast and ephitelial ovarian cancers, with HER2 receptor overexpression. Cancer Biotherapy & Radiopharmaceuticals, 37(5), 384–402. https://doi.org/10.1089/cbr.2021.0230
Mustajab, R. (2023, 28 Juni). Indonesia miliki 30.347 dokter spesialis per 27 Juni 2023. DataIndonesia.id. https://dataindonesia.id/kesehatan/detail/indonesia-miliki-30347-dokter-spesialis-per-27-juni-2023
Nelson, B. J. B., Andersson, J. D. & Wuest, F. (2021). Targeted alpha therapy: Progress in radionuclide production, radiochemistry, and applications. Pharmaceutics, 13(49). https://doi.org/10.3390/pharmaceutics13010049
Nuclear Regulatory Commission. (2011). NRC policy on release of iodine-131 therapy patients under 10 CFR 35.75 to locations other than private residences. https://www.nrc.gov/docs/ML1036/ML103620153.pdf
NRC Memorandum. (t.t.). International patient release practices following iodine-131 therapy. Diakses 20 Februari 2024, dari https://www.nrc.gov/docs/ML1421/ML14217A350.pdf
Ohnuki, K., Yoshimoto, M., & Fujii, H. (2021). Radiological protection and biological COVID-19 protection in the nuclear medicine department. European Journal of Nuclear Medicine and Molecular Imaging, 48, 6–8. https://doi.org/10.1007/s00259-020-05062-9.
Peraturan Kepala Badan Pengawas Tenaga Nuklir (Perka BAPETEN) Nomor 17 Tahun 2012 tentang Keselamatan Radiasi Dalam Kedokteran Nuklir. (2012). https://jdih.bapeten.go.id/id/dokumen/peraturan/peraturan-kepala-badan-no-17-tahun-2012-tentang-keselamatan-radiasi-dalam-kedokteran-nuklir
Peraturan Kepala Badan Riset dan Inovasi Nasional (Perka BRIN) Nomor 6 Tahun 2022 tentang Tugas, Fungsi, dan Struktur Organisasi Riset Tenaga Nuklir. (2022). https://peraturan.go.id/id/peraturan-brin-no-6-tahun-2022
Peraturan Pemerintah (PP) Nomor 45 Tahun 2023 tentang Keselamatan Radiasi Pengion dan Keamanan Zat Radioaktif. (2023).
Pharmavision (2023). Radiopharmaceuticals. Diakses 20 Maret 2024, dari https://pharmavision.health/2023/09/radiopharmaceuticals/
Poty, S., Francesconi, L.C., McDevitt, M.R., Morris, M.J. & Lewis, J.S. (2018). a-emitters for radiotherapy: From basic radiochemistry to clinical studies – Part 1. Journal of Nuclear Medicine, 59, 878–884. https://doi.org/10.2967/jnumed.116.186338
Qaim, S. M. (2001). Therapeutic radionuclides and nuclear data. Radiochimica Acta, 89(4–5), 297–302. https://doi.org/10.1524/ract.2001.89.4-5.297
Ritawidya, R., Wongso, H., Effendi, N., Pujiyanto, A., Lestari, W., Setiawan, H. & Humani, T. S. (2023). Lutetium-177-labeled prostate-specific membrance antigen-617 for molecular imaging and targeted radioligand therapy of prostate cancer. Advanced Pharmaceutical Bulletin, 13(4), 701–711. https://doi.org/10.34172/apb.2023.079
Saenger, E. L. & Kereiakes. (1980). Reflections on cancer treatment and the federal agency regulations. Radiology, 137(3), 865–866. https://doi.org/10.1148/radiology.137.3.7444073
Smart, R.C. (2014). Physics in the radiopharmacy. Dalam D. L. Bailey, J. L. Humm, A. Todd-Pokropek, A. van Aswegen. (Ed.), Nuclear medicine physics: A handbook for teachers and students. IAEA. https://www.iaea.org/publications/10368/nuclear-medicine-physics
Stella, M., Braat, A. J. A. T., van Rooij, R., de Jong, H. W. A. M. & Lam, M. G. E. H. (2022). Holmium-166 radioembolization: Current status and future perspective. Cardiovascular and Interventional Radiology, 45, 1634–1645. https://doi.org/10.1007/s00270-022-03187-y
Thomadsen, B. (2020). Radionuclide therapy events: What we can learn and what to do.
https://www.iaea.org/sites/default/files/20/07/rpop-webinar-july2020.pdf
Undang-Undang (UU) Nomor 10 Tahun 1997 tentang Ketenaganukliran. (1997). https://jdih.bapeten.go.id/id/dokumen/peraturan/undang-undang-remasyarakat-indonesia-nomor-10-tahun-1997-tentang-ketenaganukliran
United Nations Scientific Committee on the Effects of Atomic Radiation (UNSCEAR) (2022). Sources, effects and risks of ionizing radiation: UNSCEAR 2020/2021 Report to the general assembly, with scientific annexes. Volume I: Scientific Annex A. United Nations. https://www.unscear.org/unscear/en/publications/2020_2021_1.html
Yeong, C-H., Cheng, M-H. & Ng, K-H. (2014). Therapeutic radionuclides in nuclear medicine: Current and future prospects. Journal of Zhejiang University SCIENCE B (Biomed & Biotechnol), 15(10), 845–863. https://doi.org/10.1631/jzus.B1400131
Yeung, P., Pinson, J-A., Lawson, M., Leong, C. & Badawy, M. K. (2022). COVID-19 pandemic and the effect of increased utilisation of mobile X-ray examinations on radiation dose to radiographers. Journal of Medical Radiation Sciences, 69, 147–155.
https:doi.org/10.1002/jmrs.570
Downloads
Published
Series
Categories
License

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.