Indonesia Emas Berkelanjutan 2045: Kumpulan Pemikiran Pelajar Indonesia Sedunia Seri 6 Kesehatan
Keywords:
Indonesia, Tujuan Pembangunan Berkelanjutan, KesehatanSynopsis
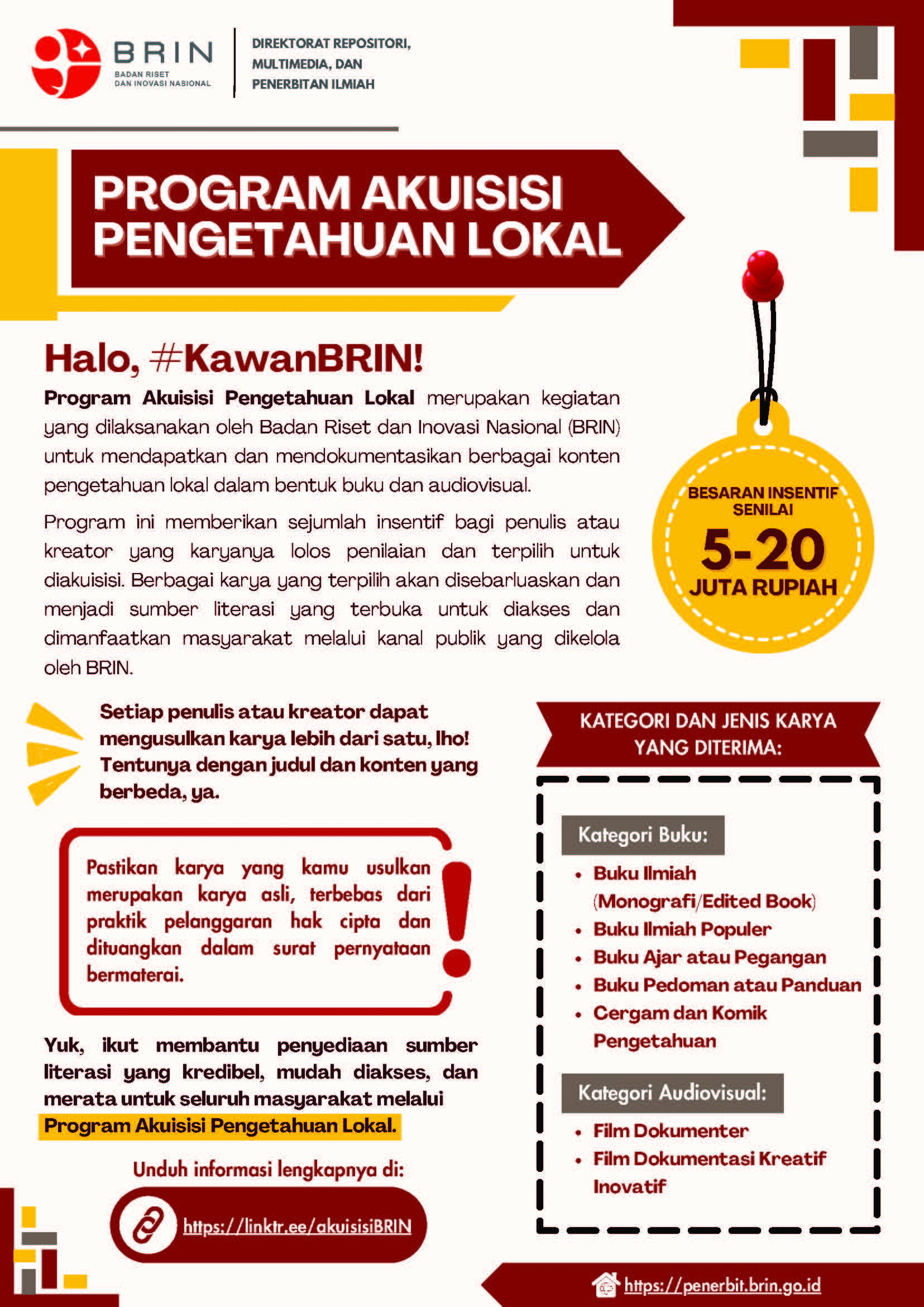
LIPI Press berkolaborasi dengan Perhimpunan Pelajar Indonesia (PPI) Dunia menerbitkan rangkaian buku seri Indonesia Emas Berkelanjutan 2045: Kumpulan Pemikiran Pelajar Indonesia Sedunia. Rangkaian bunga rampai ini terdiri dari 12 buku dengan sejumlah topik yang mendukung Tujuan Pembangunan Berkelanjutan atau Sustainable Development Goals (SDGs) untuk mencapai tujuan Indonesia Emas 2045. Buku ini merupakan seri keenam dari rangkaian tersebut. Seri Kesehatan ini secara holistik merujuk pada target ke-3 dalam SDGs, yaitu kehidupan sehat dan sejahtera, serta gagasan untuk mencapainya. Tiga tema besar yang dimuat dalam bunga rampai ini membahas perihal periode emas kehidupan, penanggulangan penyakit menular dan akibat gaya hidup, serta upaya mewujudkan sistem kesehatan berkelas dunia. Berbagai inovasi dibahas oleh para penulis dari segi sumber daya manusia, teknologi, dan pemberdayaan masyarakat. Tidak lupa prinsip ketahanan nasional dalam segi kesehatan serta keadilan juga menjadi fokus pembahasan. Kehadiran buku ini diharapkan dapat mewujudkan sistem kesehatan Indonesia yang berkelas dunia, tangguh, berkeadilan, dan adaptif menuju Indonesia Emas 2045. Harapannya setiap warga negara mendapatkan pelayanan kesehatan yang paripurna di pelosok negeri tanpa memandang status. Temukan sumbangsih pemikiran dari perwakilan pelajar Indonesia di seluruh dunia terkait perlunya kesiapan dalam menghadapi tantangan kesehatan global di masa mendatang. Selamat membaca! “Buku ini dapat menjadi salah satu referensi untuk mencapai negara maju terkait dengan aspek-aspek yang tercakup dalam Sustainable Development Goals (SDGs) dan disepakati untuk meningkatkan kualitas hidup manusia di seluruh dunia.”
Chapters
-
Pendahuluan
-
Upaya Optimalisasi Kualitas Hidup Anak Pada 1000 Hari Pertama Kehidupan (HPK)
-
Upaya Meningkatkan Status Gizi Pada Perempuan dan Anak-Anak Balita untuk Mencegah Stunting dan Wasting
-
Layanan Kesehatan Reproduksi Terpadu untuk Menurunkan Angka Kematian Ibu (AKI)
-
Menghentikan epidemi dan meningkatkan kualitas hidup penderita Tuberkulosis di Indonesia
-
Pemutusan Rantai Endemik Demam Berdarah Dengue Melalui Juru Pemantau Jentik (Jumantik)
-
Mencegah epidemi dan kematian dini akibat penyakit jantung dan paru kronis di Indonesia melalui kebijakan promotif preventif dan continuity of care didukung teknologi kesehatan
-
Strategi Pencegahan Dalam Upaya Penurunan Angka Sindrom Metabolik di Indonesia
-
Peningkatan Awareness dan Penanganan Kesehatan Mental di Indonesia
-
Strategi peningkatan keamanan pengguna jalan raya
-
Strategi Mendukung Jaminan Kesehatan Nasional yang Berkelanjutan dan Berkualitas Tinggi
-
Meningkatkan Akses Obat dan Vaksin yang Terjangkau melalui Penguatan Ekosistem Penelitian dan Pengembangan Obat
-
Upaya Tenaga Kesehatan Dalam Penurunan Risiko Gangguan Jiwa Pasca Bencana Alam Melalui Program Telepsychiatry
-
Penutup
Downloads
References
Anderson, S., Leventhal, T., & Dupara, V. (2014). Exposure to neighborhood affluence and poverty in childhood and adolescence and academic achievement and behavior. Applied Developmental Science, 18(3), 123-138.
ASEAN, UNICEF and WHO. (2016). Regional Report On Nutrition Security In Asean Volume 2. Bangkok. UNICEF. https://www.unicef.org/eapro/Regional_Report_on_Nutrition_Security_in_ASEAN_(Volume_2).pdf, diakses 2 Februari 2021
Coall, D. A., Hilbrand, S., Sear, R., & Hertwig, R. (2018). Interdisciplinary perspectives on grandparental investment: A journey towards causality. Contemporary Social Science, , 1-16.
(2), 363-395.
Bronfenbrenner, U. (1977). Toward an experimental ecology of human development. American Psychologist, 32(7), 513.
Christian, H., Zubrick, S. R., Foster, S., Giles-Corti, B., Bull, F., Wood, L., . . . Boruff, B. (2015). The influence of the neighborhood physical environment on early child health and development: A review and call for research. Health & Place, 33, 25-36.
Coall, D. A., Hilbrand, S., Sear, R., & Hertwig, R. (2018). Interdisciplinary perspectives on grandparental investment: A journey towards causality. Contemporary Social Science, , 1-16.
Daniels, S., Robson, D., Flatley, C., & Kumar, S. (2017). Demographic characteristics and pregnancy outcomes in adolescents–Experience from an australian perinatal centre. Australian and New Zealand Journal of Obstetrics and Gynaecology, 57(6), 630-635.
Finlay, J. E., Norton, M. K., & Guevara, I. M. (2017). Adolescent fertility and child health: The interaction of maternal age, parity and birth intervals in determining child health outcomes. International Journal of Child Health and Nutrition, 6(1), 16-33.
Hanushek, E. A., Kain, J. F., & Rivkin, S. G. (2004). Disruption versus tiebout improvement: The costs and benefits of switching schools. Journal of Public Economics, 88(9-10), 1721-1746.
Hatch, S. L., Frissa, S., Verdecchia, M., Stewart, R., Fear, N. T., Reichenberg, A., . . . Gazard, B. (2011). Identifying socio-demographic and socioeconomic determinants of health inequalities in a diverse london community: The south east london community health (SELCoH) study. BMC Public Health, 11(1), 861.
Irwin, L. G., Siddiqi, A., & Hertzman, G. (2007). Early child development: A powerful equalizer Human Early Learning Partnership (HELP) Vancouver, BC.
Kelleher, K. J., Boat, T. F., Houtrow, A. J., & Hoagwood, K. (2016). Poverty and supplemental security income: Can DBPs take a more active role. Journal of Developmental and Behavioral Pediatrics: JDBP, 37(4), 267.
Kementerian Kesejahteraan Rakyat RI, & Badan Perencanaan Pembangunan Nasional. (2013). Kerangka Kebijakan Gerakan 1000 Hari Pertama Kehidupan. Kemenkokesra: Jakarta.
Kemenkokesra. (2013). Pedoman Perencanaan Program Gerakan Nasional Percepatan Perbaikan Gizi dalam rangka Gerakan Seribu Hari Pertama Kehidupan (1000HPK). KemenkoKesra. Jakarta. Diakses online: https://www.bappenas.go.id/files/5013/8848/0466/PEDOMAN_SUN_10_Sept_2013.pdf
Kementerian Kesehatan Republik Indonesia. (2017). Kualitas manusia ditentukan pada 1000 hari pertama kehidupannya. Artikel publikasi,.www.kemenkes.go.id
Kementerian Kesehatan,RI. (2014). Pedoman gizi seimbang, Jakarta
Kim, T. H., Connolly, J. A., & Tamim, H. (2014). The effect of social support around pregnancy on postpartum depression among canadian teen mothers and adult mothers in the maternity experiences survey. BMC Pregnancy and Childbirth, 14(1), 162.
Lai, H. K., Berry, S. D., Verbiest, M. E., Tricker, P. J., Carr, P. E. A., Morton, S. M., & Grant, C. C. (2017). Emergency department visits of young children and long-term exposure to neighbourhood smoke from household heating–The growing up in new zealand child cohort study. Environmental Pollution, 231, 533-540.
Leventhal, T., & Newman, S. (2010). Housing and child development doi://doi.org/10.1016/j.childyouth.2010.03.008
McLachlan, E., Surjaningrum, E., Widyahening, I. S., Friska, D., Wanda, D., Fisher, J., & Arabena, K. (2018). Regional Initiatives: Building Health and Wellbeing in the First 1000 Days.
Merchant AT, Jones C, Kiure A, Kupka R, Fitzmaurice G,Hererra MG, Fawzi WW. 2003. Water and Sanitation associated with improved child growth. Eur J Clin Nutr.Vol57 (12):1562-1568
Newbury, J., Arseneault, L., Caspi, A., Moffitt, T. E., Odgers, C. L., & Fisher, H. L. (2016). Why are children in urban neighborhoods at increased risk for psychotic symptoms? findings from a UK longitudinal cohort study. Schizophrenia Bulletin, 42(6), 1372-1383.
Noonan, R. J., Boddy, L. M., Knowles, Z. R., & Fairclough, S. J. (2016). Cross-sectional associations between high-deprivation home and neighbourhood environments, and health-related variables among Liverpool children. BMJ Open, 6(1), e008693.
Oliver, J., Foster, T., Kvalsvig, A., Williamson, D. A., Baker, M. G., & Pierse, N. (2017). Risk of rehospitalisation and death for vulnerable New Zealand children. Archives of Disease in Childhood, , 312671.
Perales, F., Johnson, S. E., Baxter, J., Lawrence, D., & Zubrick, S. R. (2017). Family structure and childhood mental disorders: New findings from Australia. Social Psychiatry and Psychiatric Epidemiology, 52(4), 423-433.
Piha, K., Laaksonen, M., Martikainen, P., Rahkonen, O., & Lahelma, E. (2009). Interrelationships between education, occupational class, income and sickness absence. European Journal of Public Health, 20(3), 276-280.
Pillas, D., Marmot, M., Naicker, K., Goldblatt, P., Morrison, J., & Pikhart, H. (2014). Social inequalities in early childhood health and development: A european-wide systematic review. Pediatric Research, 76(5), 418.
Power, C., Kuh, D., & Morton, S. (2013). From developmental origins of adult disease to life course research on adult disease and aging: Insights from birth cohort studies. Annual Review of Public Health, 34, 7-28.
Putri,D.S, Sukandar,D. (2012). Keadaan rumah, kebiasaan makan, status gizi, dan status kesehatan balita diKecamatan Tamansari, Kabupaten Bogor. JurnalGiziPangan.Vol7(3):163-168.
Rahayu, A., dan Khairiyati, L. (2014). Risiko Pendidikan Ibu Terhadap Kejadian Stunting Pada Anak 6-23 Bulan.Jurnal Penelitian Gizi Makanan.Vol. 37 (2): 129-136
Reynolds, S. A., Fernald, L. C., Deardorff, J., & Behrman, J. R. (2017). Family structure and child development in Chile: A longitudinal analysis of household transitions involving fathers and grandparents
Sudargo, T., & Aristasari, T. (2018). 1000 hari pertama kehidupan. UGM PRESS.
Sumarmi, S., & Sumarmi, S. (2017). Tinjauan Kritis Intervensi Multi Mikronutrien pada 1000 Hari Pertama Kehidupan. Nutrition and Food Research, 40(1), 17-28.
Tim Nasional Percepatan Penanggulangan Kemiskinan. (2017). 100 Kabupaten/Kota Prioritas Untuk Intervensi Anak Kerdil( Stunting). Jakarta Pusat. Sekretariat Wakil Presiden Indonesia.
UKAID. 2011. Scalling Up Nutrition: The UK’s position paper on undernutrition. Departement of International Development.
USAID.2014. Multi-sectoral Nutrition Strategy 2014-2025Technical Guidance Brief: Implementation Guidance for Ending Preventable Maternal and Child Death.Hal1-6.
Whayne, T. F. (2015). Epigenetics in the development, modification, and prevention of cardiovascular disease. Molecular Biology Reports, 42(4), 765-776.
WHO. 2005. Nutrition and Adolescence: Issues and Challenges for the Health Sector. Geneva: WHO Press.
World Bank. 2006. Repositioning nutrition as central development astrategy for large scale action[Internet]. Geneva: WorldBank; 2006. Diakses pada tanggal 2 Feburai 2021.Tersedia di http://www.unhcr.org/45f6c4432. pdf.
Zhang, Y., & Ren, J. (2016). Epigenetics and obesity cardiomyopathy: From pathophysiology to prevention and management. Pharmacology & therapeutics, 161, 52-66.
Bappenas. (2012). Kerangka Kebijakan - Gerakan Nasional Percepatan Perbaikan Gizi Dalam Rangka Seribu Hari Pertama Kehidupan (Gerakan 1000 HPK). https://www.bappenas.go.id/files/7713/8848/0483/KERANGKA_KEBIJAKAN_-_10_Sept_2013.pdf
British Nutrition Foundation. (2016). Fortification. https://www.nutrition.org.uk/nutritionscience/foodfacts/fortification.html?start=2
Ciresi, A., & Giordano, C. (2017). Vitamin D across growth hormone (GH) disorders: From GH deficiency to GH excess. In Growth Hormone and IGF Research. https://doi.org/10.1016/j.ghir.2017.02.002
Cusick, S., & Georgieff, M. K. (n.d.). The first 1,000 days of life: The brain’s window of opportunity. Retrieved January 24, 2021, from https://www.unicef-irc.org/article/958-the-first-1000-days-of-life-the-brains-window-of-opportunity.html
Doku, D. T., Bhutta, Z. A., & Neupane, S. (2020). Associations of women’s empowerment with neonatal, infant and under-5 mortality in low-and /middle-income countries: meta-analysis of individual participant data from 59 countries. BMJ Global Health. https://doi.org/10.1136/bmjgh-2019-001558
Hug, L., Lee, S., Liu, Y., Mishra, A., Sharrow, D., You, D., Cao, B., Ho, J., Louise Strong World Bank Group Emi Suzuki, K., Andreev, K., Bassarsky, L., Gaigbe-Togbe, V., Gerland, P., Gu, D., Hertog, S., Li, N., Spoorenberg, T., Ueffing, P., Wheldon, M., … Wakefield, J. (2020). Levels & Trends in Child Mortality - Report 2020.
Kemenkes RI. (2016). Program Indonesia Sehat dengan Pendekatan Keluarga. Kemenkes RI. https://www.kemkes.go.id/article/print/17070700004/program-indonesia-sehat-dengan-pendekatan-keluarga.html
Kemenkes RI. (2020). Pedoman Indikator Program Kesmas dalam RPJMN dan Renstra Tahun 2020-2024. https://kesmas.kemkes.go.id/assets/uploads/contents/attachments/ef5bb48f4aaae60ebb724caf1c534a24.pdf
Mahmudiono, T., Sumarmi, S., & Rosenkranz, R. R. (2017). Household dietary diversity and child stunting in East Java, Indonesia. Asia Pacific Journal of Clinical Nutrition. https://doi.org/10.6133/apjcn.012016.01
Nurhayati, E., Paramashanti, B. A., Astiti, D., & Aji, A. S. (2020). Dietary diversity, vitamin D intake and childhood stunting: A case-control study in Bantul, Indonesia. Malaysian Journal of Nutrition. https://doi.org/10.31246/MJN-2020-0021
Oktaria, V., Graham, S. M., Triasih, R., Soenarto, Y., Bines, J. E., Ponsonby, A. L., Clarke, M. W., Dinari, R., Nirwati, H., & Danchin, M. (2020). The prevalence and determinants of vitamin D deficiency in indonesian infants at birth and six months of age. PLoS ONE. https://doi.org/10.1371/journal.pone.0239603
Schwarzenberg, S. J., & Georgieff, M. K. (2018). Advocacy for improving nutrition in the first 1000 days to support childhood development and adult health. Pediatrics. https://doi.org/10.1542/peds.2017-3716
Subandi, S., Watson, F., Sukotjo, S., Jee, H. R., & Maruti, A. K. (2019). Pembangunan Gizi Di indonesia. Bappenas. https://www.bappenas.go.id/files/1515/9339/2047/FA_Preview_HSR_Book04.pdf
Survey, H. (2017). Causes of Death in Children Under 5 Years of Age - Indonesia. 1–13. https://ourworldindata.org/grapher/causes-of-death-in-children-under-5?country=~IDN
Transforming Our World: The 2030 Agenda for Sustainable Development. (2018). In A New Era in Global Health. https://doi.org/10.1891/9780826190123.ap02
Walson, J. L., & Berkley, J. A. (2018). The impact of malnutrition on childhood infections. In Current Opinion in Infectious Diseases. https://doi.org/10.1097/QCO.0000000000000448
World Bank. (2019). Indonesia | Data. https://data.worldbank.org/country/ID
World Health Assembly. (2012). Proposed Global Target For Maternal, Infant and Young Child Nutrition.
World Health Organization. (2020). Malnutrition. https://www.who.int/news-room/q-a-detail/malnutrition
Ayu, M. D., Rifai, A., & Liesmayani, E. E. (2020). Analisis pemanfaatan pelayanan kesehatan peduli remaja (pkpr) di wilayah kerja puskesmas langsa kota tahun 2020. Journal of healthcare technology and medicine, 6(2), 1127-1141.
Chalid, M. T. (2017). Upaya menurunkan Angka Kematian Ibu: peran petugas kesehatan. Departemen Obstetri dan Ginekologi. Fakultas Kedokteran. Unhas. PT. Gakken. diakses, 19, 59.
Chasanah, S. U. (2017). Peran Petugas Kesehatan Masyarakat dalam Upaya Penurunan Angka Kematian Ibu Pasca MDGs 2015. Jurnal kesehatan masyarakat Andalas, 9(2), 73-79.
Emilia, O., & Prabandari, Y. S. (2019). Promosi kesehatan dalam lingkup kesehatan reproduksi. UGM PRESS.
Helmizar, H. (2014). Evaluasi Kebijakan Jaminan Persalinan (Jampersal) Dalam Penurunan Angka Kematian Ibu Dan Bayi Di Indonesia. KEMAS: Jurnal Kesehatan Masyarakat, 9(2), 197-205.
Indonesia, S. (2016). Profile of the People of Indonesia, Supas Result 2015 (6024380275).
Jalilah, N. H., & Prapitasari, R. (2021). KESEHATAN REPRODUKSI DAN KELUARGA BERENCANA. Penerbit Adab.
Kemenkes, R. (2016). Profil kesehatan Indonesia tahun 2015. Jakarta: Kementerian Kesehatan Republik Indonesia.
Maryani, D., & Nainggolan, R. R. E. (2019). Pemberdayaan masyarakat. Deepublish.
Pulungan, P. W., Rusmini, R., Zuheriyatun, F., Faizah, S. N., Kurniasih, H., Winarso, S. P., Aini, F. N., Amalia, R., Lubis, R. I. P., & Utami, V. N. (2020). Teori Kesehatan Reproduksi. Yayasan Kita Menulis.
Saputra, W., Fanggidae, V., & Mafthuchan, A. (2013). Efektivitas kebijakan daerah dalam penurunan angka kematian ibu dan bayi. Kesmas: Jurnal Kesehatan Masyarakat Nasional (National Public Health Journal), 7(12), 531-537.
Say, L., Chou, D., Gemmill, A., Tunçalp, Ö., Moller, A.-B., Daniels, J., Gülmezoglu, A. M., Temmerman, M., & Alkema, L. (2014). Global causes of maternal death: a WHO systematic analysis. The Lancet global health, 2(6), e323-e333.
Setyani, R. A. (2020). Serba-Serbi Kesehatan Reproduksi Wanita dan Keluarga Berencana. PT. SAHABAT ALTER INDONESIA.
Situmorang, A. (2016). Pelayanan kesehatan reproduksi remaja di puskesmas: isu dan tantangan. Jurnal Kependudukan Indonesia, 6(2), 21-32.
Soedarmono, Y. (2017). The Indonesian approach to reduce maternal mortality. ISBT Science Series, 12(1), 272-280.
Sulaeman, E. S. (2012). Pemberdayaan Masyarakat di Bidang Kesehatan. Teori dan Implementasi, Gajah Mada University Press, Yokyakarta.
Peraturan Presiden Republik Indonesia Nomor 72 Tahun 2012 Tentang Sistem Kesehatan Nasional
Alene, K. A., Wangdi, K., & Clements, A. C. A. (2020). Impact of the COVID-19 Pandemic on Tuberculosis Control: An Overview. Tropical Medicine and Infectious Disease, 5(3), 123. https://doi.org/10.3390/tropicalmed5030123
Centers for Disease Control and prevention. (2008). Tuberculosis Genotyping. TB Elimination.
Chiang, C. Y., Islam, T., Xu, C., Chinnayah, T., Garfin, A. M. C., Rahevar, K., & Raviglione, M. (2020). The impact of COVID-19 and the restoration of tuberculosis services in the Western Pacific Region. In European Respiratory Journal. https://doi.org/10.1183/13993003.03054-2020
Chughtai, A. A., Seale, H., & MacIntyre, C. R. (2020). Effectiveness of Cloth Masks for Protection against Severe Acute Respiratory Syndrome Coronavirus 2. Emerging Infectious Diseases, 26(10). https://doi.org/10.3201/EID2610.200948
Churchyard, G., Kim, P., Shah, N. S., Rustomjee, R., Gandhi, N., Mathema, B., Dowdy, D., Kasmar, A., & Cardenas, V. (2017). What We Know about Tuberculosis Transmission: An Overview. Journal of Infectious Diseases, 216(6), 629–635. https://doi.org/10.1093/infdis/jix362
Cucunawangsih, Wiwing, V., Widysanto, A., & Lugito, N. P. H. (2015). Mycobacterium tuberculosis resistance pattern against first-line drugs in patients from urban area. International Journal of Mycobacteriology. https://doi.org/10.1016/j.ijmyco.2015.08.002
Heemskerk D, et al. (2015). Pathogenesis. In Tuberculosis in Adults and Children. Springer. https://www.ncbi.nlm.nih.gov/books/NBK344406/
Hopewell, P. C., Reichman, L. B., & Castro, K. G. (2021). Parallels and Mutual Lessons in Tuberculosis and COVID-19 Transmission, Prevention, and Control. Emerging Infectious Diseases, 27(3). https://doi.org/10.3201/eid2703.203456
Jenkins, C., & Sunjaya, A. (2021). Social distancing as a strategy to prevent respiratory virus infections. Respirology, 26, 143–144. https://doi.org/10.1111/resp.13990
Jones, N. R., Qureshi, Z. U., Temple, R. J., Larwood, J. P. J., Greenhalgh, T., & Bourouiba, L. (2020). Two metres or one: what is the evidence for physical distancing in covid-19? BMJ (Clinical Research Ed.). https://doi.org/10.1136/bmj.m3223
Kemenkes RI. (2016). Situasi Imunisasi di Indonesia.
Kemenkes RI. (2018). Infodatin Tuberkulosis. In Kementerian Kesehatan RI.
McHenry, M. L., Williams, S. M., & Stein, C. M. (2020). Genetics and evolution of tuberculosis pathogenesis: New perspectives and approaches. Infection, Genetics and Evolution. https://doi.org/10.1016/j.meegid.2020.104204
Meijers, A. S., Troost, R., Ummels, R., Maaskant, J., Speer, A., Nejentsev, S., Bitter, W., & Kuijl, C. P. (2020). Efficient genome editing in pathogenic mycobacteria using Streptococcus thermophilus CRISPR1-Cas9. Tuberculosis, 124. https://doi.org/10.1016/j.tube.2020.101983
Mesfin, Y. M., Hailemariam, D., Biadglign, S., & Kibret, K. T. (2014). Association between HIV/AIDS and multi-drug resistance tuberculosis: A systematic review and meta-analysis. PLoS ONE, 9(2). https://doi.org/10.1371/journal.pone.0082235
Migliori, G. B., Tiberi, S., Zumla, A., Petersen, E., Chakaya, J. M., Wejse, C., Torrico, M. M., Duarte, R., Alffenaar, J. W., Schaaf, H. S., Marais, B. J., Cirillo, D. M., Alagna, R., Rendon, A., Pontali, E., Piubello, A., Figueroa, J., Ferlazzo, G., García-Basteiro, A., … Zellweger, J. P. (2020). MDR/XDR-TB management of patients and contacts: Challenges facing the new decade. The 2020 clinical update by the Global Tuberculosis Network. International Journal of Infectious Diseases. https://doi.org/10.1016/j.ijid.2020.01.042
Narasimhan, P., Wood, J., Macintyre, C. R., & Mathai, D. (2013). Risk factors for tuberculosis. In Pulmonary Medicine. https://doi.org/10.1155/2013/828939
Peeples, L. (2020). Face masks: what the data say. In Nature. https://doi.org/10.1038/d41586-020-02801-8
Pradipta, I. S., Forsman, L. D., Bruchfeld, J., Hak, E., & Alffenaar, J. W. (2018). Risk factors of multidrug-resistant tuberculosis: A global systematic review and meta-analysis. Journal of Infection, 77, 469–478. https://doi.org/10.1016/j.jinf.2018.10.004
Safar, H. A., Mustafa, A. S., & McHugh, T. D. (2020). COVID-19 vaccine development: What lessons can we learn from TB? Annals of Clinical Microbiology and Antimicrobials, 19, 56. https://doi.org/10.1186/s12941-020-00402-x
Sari, N. I. P., Mertaniasih, N. M., Soedarsono, & Maruyama, F. (2019). Application of serial tests for Mycobacterium tuberculosis detection to active lung tuberculosis cases in Indonesia. BMC Research Notes, 12(313). https://doi.org/10.1186/s13104-019-4350-9
Subastian, B. (2020). INFOGRAFIS: Cara Taiwan Suplai Masker untuk Semua Warga. cnnindonesia.com/internasional/20200406164133-116-490862/infografis-cara-taiwan-suplai-masker-untuk-semua-warga
Sunjaya, A. P., & Jenkins, C. (2020). Rationale for universal face masks in public against COVID-19. In Respirology. https://doi.org/10.1111/resp.13834
Sunjaya, A. P., & Morawska, L. (2020). Evidence Review and Practice Recommendation on the Material, Design, and Maintenance of Cloth Masks. Disaster Medicine and Public Health Preparedness, 14(5), 42–46. https://doi.org/10.1017/dmp.2020.317
Tegegne, B. S., Habtewold, T. D., Mengesha, M. M., & Burgerhof, J. G. M. (2018). Association between diabetes mellitus and multi-drug-resistant tuberculosis: A protocol for a systematic review and meta-analysis. Systematic Reviews, 7(161). https://doi.org/10.1186/s13643-017-0407-9
The Lancet Infectious Diseases. (2021). Tuberculosis and malaria in the age of COVID-19. In The Lancet Infectious Diseases. https://doi.org/10.1016/S1473-3099(20)30946-4
Whitlow, E., Mustafa, A. S., & Hanif, S. N. M. (2020). An overview of the development of new vaccines for tuberculosis. Vaccines, 8, 586. https://doi.org/10.3390/vaccines8040586
WHO. (2020). Global Tuberculosis Report 2020.
WHO Global TB Programme. (2018). The use of next-generation sequencing technologies for the detection of mutations associated with drug resistance in Mycobacterium tuberculosis complex: technical guide. In WHO Global TB Programme.
Yan, M. Y., Li, S. S., Ding, X. Y., Guo, X. P., Jin, Q., & Sun, Y. C. (2020). A crispr-assisted nonhomologous end-joining strategy for efficient genome editing in Mycobacterium tuberculosis. MBio, 11(1), e02364-19. https://doi.org/10.1128/mBio.02364-19
Adnan, A. B., & Siswani, S. (2019). Peran Kader Jumantik Terhadap Perilaku Masyarakat Dalam Upaya Pencegahan Penyakit Demam Berdarah Dengue (Dbd) Di Wilayah Kerja Kelurahan Tebet Timur Tahun 2019. JUKMAS: Jurnal Untuk Masyarakat Sehat, 3(2), 204-218.
Amira, I., Hendrawati, H., & Senjaya, S. (2019). Perilaku Masyarakat Dalam Upaya Pencegahan Penyakit Demam Berdarah (Dbd) Melalui Metode Pemberantasan Sarang Nyamuk (Psn) Di Desa Karyalaksana Kecamatan Ibun Kabupaten Bandung. Jurnal Kesehatan Bakti Tunas Husada: Jurnal Ilmu-ilmu Keperawatan, Analis Kesehatan dan Farmasi, 19(2), 169-177.
Brady, O. J., & Hay, S. I. (2020). The global expansion of dengue: how Aedes aegypti mosquitoes enabled the first pandemic arbovirus. Annual review of entomology, 65, 191-208.
Candra, A. (2010). Demam Berdarah Dengue: Epidemiologi, Patogenesis, dan Faktor Risiko Penularan. Aspirator Journal of Vector-Borne Diseases, 2(2), 53636.
Direktorat Jenderal Pengendalian dan Pencegahan Penyakit, (2016), Petunjuk Teknis Implementasi PSN 3M - Plus Dengan Gerakan 1 Rumah 1 Jumantik.
Hidayat, W. A., Yaswir, R., & Murni, A. W. (2017). Hubungan jumlah trombosit dengan nilai hematokrit pada penderita demam berdarah dengue dengan manifestasi perdarahan spontan di RSUP Dr. M. Djamil Padang. Jurnal Kesehatan Andalas, 6(2), 446-451.
Kementerian Kesehatan RI. 2018. Info Datin Situasi Demam Berdarah Dengue (DBD)
Kementerian Kesehatan RI (2019). https://sehatnegeriku.kemkes.go.id/baca/rilis-media/20190129/3629259/satu-rumah-satu-jumantik-efektif-cegah-dbd/
Kementerian Kesehatan RI (2020). https://sehatnegeriku.kemkes.go.id/baca/umum/20201203/2335899/data-kasus-terbaru-dbd-indonesia/
Mubarokah, R., & KM, S. I. S. (2013). Upaya Peningkatan Angka Bebas Jentik (ABJ) DBD Melalui Penggerakan Jumantik. Unnes Journal of Public Health, 2(3).
Parulian Manalu, H. S., & Munif, A. (2016). Pengetahuan dan perilaku masyarakat dalam pencegahan Demam Berdarah Dengue di Provinsi Jawa Barat dan Kalimantan Barat. Aspirator Journal of Vector-Borne Diseases, 8(2), 69-76.
Pratamawati, D. A. (2012). Peran juru pantau jentik dalam sistem kewaspadaan dini demam berdarah dengue di Indonesia. Kesmas: Jurnal Kesehatan Masyarakat Nasional (National Public Health Journal), 6(6), 243-248.
Priesley, F., Reza, M., & Rusdji, S. R. (2018). Hubungan perilaku pemberantasan sarang nyamuk dengan menutup, menguras dan mendaur ulang plus (PSN M Plus) terhadap kejadian demam berdarah dengue (DBD) di kelurahan andalas. Jurnal Kesehatan Andalas, 7(1), 124-130.
Rakhmani, A. N., Limpanont, Y., Kaewkungwal, J., & Okanurak, K. (2018). Factors associated with dengue prevention behaviour in Lowokwaru, Malang, Indonesia: a cross-sectional study. BMC Public Health, 18(1), 619. https://doi.org/10.1186/s12889-018-5553-z
Rini, W. N. E., & Ningsih, V. R. (2020). UPAYA PENCEGAHAN DBD DENGAN GERAKAN SATU RUMAH SATU JUMANTIK DALAM MEWUJUDKAN MASYARAKAT PEDULI SEHAT. Jurnal Salam Sehat Masyarakat (JSSM), 2(1), 49-55.
Salim, M., Ambarita, L. P., Margarethy, I., Nurmaliani, R., & Ritawati, R. (2020). Pelaksanaan gerakan satu rumah satu jumantik (g1r1j) dengan pola pendampingan terhadap pengetahuan, sikap dan tindakan masyarakat dalam di kota jambi. Jurnal ekologi kesehatan, 19(3), 196-210.
Sukesi, T. W., Mulasari, S. A., & Sulistyawati, S. (2019). Penguatan jumantik di Patukan, Gamping, Sleman. Seminar Nasional Hasil Pengabdian Kepada Masyarakat,
Sukohar, A. (2014). Demam Berdarah Dengue (DBD). Jurnal Medula, 2(02).
Yunita, D. S. (2016). Hubungan antara Pelatihan, Motivasi dan Ketersediaan Fasilitas dengan Partisipasi Jumantik di Kota Blitar. Indones J Public Heal, 11(1), 40-50.
Anderson, I., Meliala, A., Marzoeki, P., & Pambudi, E. (2014). The Production, Distribution, and Performance of Physicians, Nurses, and Midwives in Indonesia: An Update. Retrieved from
Bashshur, R. L., Shannon, G. W., & Smith, B. R. (2014). The Empirical Foundations of Telemedicine Interventions for Chronic Disease Management. Telemedicine and e-Health, 20(9).
Batsis, J. A., Pletcher, S. N., & Stahl, J. E. (2017). Telemedicine and primary care obesity management in rural areas – innovative approach for older adults? BMC Geriatr, 17(6).
Boydell, K. M., Hodgins, M., Pignatiello, A., Teshima, J., Edwards, H., & Willis, D. (2014). Using technology to deliver mental health services to children and youth: a scoping review. J Can Acad Child Adolesc Psychiatr, 23.
Carrion, C., Arroyo, M. L., Castell, C., Puigdomenech, E., Felipe Gomez, S., Domingo, L., & Espallargues, M. (2016). Use of the Smartphone to Promote Healthy Habits among Teen-agers, Spain. Rev Esp Salud Publica, 90.
Coe, G., & de Beyer, J. (2014). The imperative for health promotion in universal health coverage. Glob Health Sci Pract, 2(1).
Cordova, F. C., Ciccolella, D., Grabianowski, C., Gaughan, J., Brennan, K., Goldstein, F., . . . Criner, G. J. (2016). A Telemedicine-Based Intervention Reduces the Frequency and Severity of COPD Exacerbation Symptoms: A Randomized, Controlled Trial. Telemedicine and e-Health, 22(2).
Efendi, F. (2012). Health worker recruitment and deployment in remote areas of Indonesia. Rural and Remote Health, 12.
Guinto, R. L., Curran, U. Z., Suphanchaimat, R., & Pocock, N. S. (2015). Universal health coverage in 'One ASEAN': are migrants included? Global health action, 8.
Hootsuite. (2020). Digital 2020: Indonesia. Retrieved from https://www.slideshare.net/DataReportal/digital-2020-indonesia-january-2020-v01?ref=https://datareportal.com/
internal, D. (2015). Kondisi ketenagaan di Puskesmas tahun 2015. In.
Investments, I., eMarketer, & APJII (Producer). (2016). Indonesia Has 100 Million Internet Users, Internet Penetration at 40%. Retrieved from http://www.indonesia-investments.com/news/todays-headlines/indonesia-has-100-million-internet-users-internet-penetration-at-40/item6827?
Kesehatan, K. (2013). Analisis Kebutuhan Tenaga Kesehatan Sebagai Dasar Untuk Pengembangan Prodi Pendidikan Nakes. Retrieved from Batam:
Kesehatan, K. (Producer). (2016a). Namun Dibayar Total Melalui Uang Kapitasi Sampai 734 Juta per Bulan untuk Satu Puskesmas. Retrieved from http://kliping.depkes.go.id/upload/f7d2d4bdae6fada6b2cd3d902ee3148b.pdf
Kesehatan, K. (2016b). Profil Kesehatan Indonesia 2015. Retrieved from Jakarta:
Kesehatan, M. (2014). Peraturan Menteri Kesehatan (PMK) No. 75 tahun 2014 In.
Laranjo, L., Arguel, A., Neves, A. L., Gallagher, A. M., Kaplan, R., & Mortimer, N. (2015). The influence of social networking sites on health behavior change: a systematic review and meta-analysis. J Am Med Inform Assoc, 22.
Murray, C. J. L., Aravkin, A. Y., Zheng, P., Abbafati, C., Abbas, K. M., Abbasi-Kangevari, M., . . . Lim, S. S. (2020). Global burden of 87 risk factors in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. The Lancet, 396(10258), 1223-1249. doi:https://doi.org/10.1016/S0140-6736(20)30752-2
Okezone (Producer). (2012). Mengintip Teknologi Mobil Unit Bencana Kominfo. Retrieved from http://techno.okezone.com/read/2012/06/05/56/641627/mengintip-teknologi-mobil-tanggap-bencana-besutan-kominfo/large
Priyatmoko, H., Lazuardi, M. K., & Hasanbasri, M. A. (2014). Analisis Determinan Ketersediaan Dokter Spesialis dan Gambaran Fasilitas Kesehatan di RSU Pemerintah Kabupaten/Kota Indonesia (Analisis Data Rifaskes 2011). Retrieved from
Pusat Data dan Informasi Kementerian Kesehatan. (2016). Buletin Jendela Data & Informasi Kesehatan. Retrieved from Jakarta:
Quinonez, S. G., Walthouwer, M. J. L., Schulz, D. N., & de Vries, H. (2016). mHealth or eHealth? Efficacy, Use, and Appreciation of a Web-Based Computer-Tailored Physical Activity Intervention for Dutch Adults: A Randomized Controlled Trial. J Med Internet Res, 18(11).
RI, M. K. (November 2016). Kerja Nyata Sehatkan Indonesia Membangun Integritas dan Pencegahan Korupsi di Sektor Kesehatan. In.
Rokx, C., Giles, J., Satriawan, E., Marzoeki, P., & Harimurti, P. (2014). New Insight into the Provision of Health Services in Indonesia: A Health Workforce Study. Directions in Development.
Russo, J. E., McCool, R. R., & Davies, L. (2016). VA telemedicine: an analysis of cost and time savings. Telemed J E Health, 22(3).
Sagarra, S. E. (Producer). (2015). Georgia Aims to Revive Its Rural Healthcare System. Retrieved from http://www.ihexecutive.com/patient-care/clinical-pathways/article/12077407/georgia-aims-to-revive-its-rural-healthcare-system
Schulz, D. N., Kremers, S. P., Vandelanotte, C., van Adrichem, M. J., Schneider, F., Candel, M. J., & de Vries , H. (2014). Effects of a web-based tailored multiple-lifestyle intervention for adults: a two-year randomized controlled trial comparing sequential and simultaneous delivery modes. J Med Internet Res, 16(1).
Smith, H. S., Criner, A. J., Fehrle, D., Grabianowski, C. L., Jacobs, M. R., & Criner, G. J. (2016). Use of a SmartPhone/Tablet-Based Bidirectional Telemedicine Disease Management Program Facilitates Early Detection and Treatment of COPD Exacerbation Symptoms. Telemedicine and e-Health, 22(5).
Storm, V., Dorenkamper, J., Reinwand, D. A., Wienert, J., de Vries, H., & Lippke, S. (2016). Effectiveness of a Web-Based Computer-Tailored Multiple-Lifestyle Intervention for People Interested in Reducing their Cardiovascular Risk: A Randomized Controlled Trial. J Med Internet Res, 18(4).
Sunjaya, A. P., & Sunjaya, A. F. (2018). Diabetes in pregnancy and infant mortality: link with glycemic control. Diabetes & Metabolic Syndrome: Clinical Research & Reviews, 12(6), 1031-1037.
Sunjaya, A. P., Sunjaya, A. F., & Priyana, A. (2019). Insights and challenges of indonesia’s acute coronary syndrome telecardiology network: three year experience from a single center and in west Jakarta, Indonesia. IOP Conference Series: Materials Science and Engineering, 508, 012142. doi:10.1088/1757-899x/508/1/012142
Suwandono, A., Muharso, Achadi, A., & Aryastami, K. (2015). Human Resources on Health(HRH) for foreign countries: A case of doctor 'deficit' in indonesia. Retrieved from
WHO. (2012). National eHealth strategy toolkit: International Telecommunication Union.
WHO. (2014). Noncommunicable Diseases Country Profiles 2014. Retrieved from
WHO (Producer). (2017). Health promotion and disease prevention through population-based interventions, including action to address social determinants and health inequity. Retrieved from http://www.emro.who.int/about-who/public-health-functions/health-promotion-disease-prevention.html
WHO. (2020). Country statistics and global health estimates. Retrieved from http://www.who.int/gho/countries/idn.pdf?ua=1
Widyantoro, B., Situmorang, T. D., Turana, Y., Barack, R., Delliana, J., Roesli, R. M. A., . . . Santoso, A. (2019). May Measurement Month 2017: an analysis of the blood pressure screening campaign results in Indonesia-South-East Asia and Australasia. Eur Heart J Suppl, 21(Suppl D), D63-d65. doi:10.1093/eurheartj/suz057
Ariani, Y., Soeharso, P., & Sjarif, D. R. (2017). Genetics and genomic medicine in Indonesia. Molecular Genetics and Genomic Medicine. https://doi.org/10.1002/mgg3.284
Bappenas. (2017). Metadata Indikator Tujuan Berkelanjutan (TPB)/Sustainable Development Goals (SDGs) Indonesia. http://sdgs.bappenas.go.id/pilar-sosial/
Bappenas. (2019a). Roadmap of SDGs Indonesia. https://www.unicef.org/indonesia/media/1626/file/Roadmap of SDGs.pdf
Bappenas. (2019b). Transisi Demografi dan Epidemiologi: Permintaan Pelayanan Kesehatan di Indonesia. https://www.bappenas.go.id/files/8515/9339/1872/FA_Preview_HSR_Book01.pdf
Baumgart, M., Snyder, H.M., Carrillo, M.C., Fazio, S., Kim, H. & Johns, H. 2015, 'Summary of the evidence on modifiable risk factors for cognitive decline and dementia: a population-based perspective', Alzheimer's & Dementia, vol. 11, no. 6, pp. 718-26.
Bhupathiraju, S. N., & Hu, F. B. (2016). Epidemiology of obesity and diabetes and their cardiovascular complications. Circulation Research. https://doi.org/10.1161/CIRCRESAHA.115.306825
Börnhorst, C., Russo, P., Veidebaum, T., Tornaritis, M., Molnár, D., Lissner, L., Mårild, S., De Henauw, S., Moreno, L. A., Floegel, A., Ahrens, W., & Wolters, M. (2020). The role of lifestyle and non-modifiable risk factors in the development of metabolic disturbances from childhood to adolescence. International Journal of Obesity. https://doi.org/10.1038/s41366-020-00671-8
Christijani, R. (2019). Penentuan Diagnosis Sindrom Metabolik Berdasarkan Penilaian Skor Sindrom Metabolik dan NCEP ATP-III pada Remaja [Penelitian di Beberapa SMA di Kota Bogor]. Penelitian Gizi Dan Makanan (The Journal of Nutrition and Food Research), 42(1), 21–28. https://doi.org/10.22435/pgm.v42i1.2418
Di Sanzo, M., Cipolloni, L., Borro, M., La Russa, R., Santurro, A., Scopetti, M., Simmaco, M., & Frati, P. (2017). Clinical Applications of Personalized Medicine: A New Paradigm and Challenge. Current Pharmaceutical Biotechnology. https://doi.org/10.2174/1389201018666170224105600
Dirjen P2PTM. (2019). Strategi Pencegahan dan Pengendalian PTM di Indonesia - Direktorat P2PTM. Retrieved August 17, 2020, from http://www.p2ptm.kemkes.go.id/profil-p2ptm/latar-belakang/strategi-pencegahan-dan-pengendalian-ptm-di
Doestzada, M., Vila, A. V., Zhernakova, A., Koonen, D. P. Y., Weersma, R. K., Touw, D. J., Kuipers, F., Wijmenga, C., & Fu, J. (2018). Pharmacomicrobiomics: a novel route towards personalized medicine? In Protein and Cell. https://doi.org/10.1007/s13238-018-0547-2
IDAI. (2014). Diagnosis dan Tata Laksana Sindrom Metabolik pada Anak dan Remaja. http://spesialis1.ika.fk.unair.ac.id/wp-content/uploads/2017/03/Konsensus-Diagnosis-dan-Tata-Laksana-Sindrom-Metabolik-Pada-Anak-dan-Remaja.pdf
Joy, T., Lahiry, P., Pollex, R. L., & Hegele, R. A. (2008). Genetics of metabolic syndrome. In Current Diabetes Reports. https://doi.org/10.1007/s11892-008-0025-y
Kataria, I., Chadha, R., & Pathak, R. (2015). Metabolic syndrome in adults: relation with diet and other lifestyle factors. Reviews in Health Care, 6(3), 99–124. https://doi.org/10.7175/rhc.v6i3.1188
Kemendikbud. (2017). Peta Jalan Generasi Emas Indonesia 2045. In Kementerian Pendidikan dan Kebudayaan Republik Indonesia. https://paska.kemdikbud.go.id/wp-content/uploads/2018/08/170822-V.2-Generasi-Emas-2045-.pdf
Lim, M. A., Huang, I., Yonas, E., Vania, R., & Pranata, R. (2020). A wave of non-communicable diseases following the COVID-19 pandemic. Diabetes and Metabolic Syndrome: Clinical Research and Reviews. https://doi.org/10.1016/j.dsx.2020.06.050
Marc, J. (2007). Genetic Succeptibility to Metabolic Syndrome. EJIFCC, 18(1), 7–14.
Misra, A., Misra, R., Wijesuriya, M., & Banerjee, D. (2007). The metabolic syndrome in South Asians: Continuing escalation & possible solutions. In Indian Journal of Medical Research.
Monda, K. L., North, K. E., Hunt, S. C., Rao, D. C., Province, M. A., & Kraja, A. T. (2010). The genetics of obesity and the metabolic syndrome. Endocrine, Metabolic & Immune Disorders Drug Targets, 10(2), 86–108.
Nurjanah, F. K. R. (2015). Gaya Hidup dan Kejadian Sindrom Metabolik pada Karyawan. Jurnal Gizi Pangan, 10(1), 17–24.
Pan, W. H., Yeh, W. T., & Weng, L. C. (2008). Epidemiology of metabolic syndrome in Asia. Asia Pacific Journal of Clinical Nutrition, 17(S1), 37–42. https://doi.org/10.11320/ningendock2005.21.1110
Parikh, R., & Mohan, V. (2012). Changing definitions of metabolic syndrome. Indian Journal of Endocrinology and Metabolism, 16(1), 7–12. https://doi.org/10.4103/2230-8210.91175
Park, S.K. & Larson, J.L. 2014, 'The relationship between physical activity and metabolic syndrome in people with chronic obstructive pulmonary disease', The Journal of cardiovascular nursing, vol. 29, no. 6, pp. 499-507.
Peraturan Menteri Kesehatan Republik Indonesia Nomor 30 Tahun 2013 tentang Pencantuman Informasi Kandungan Gula, Garam, dan Lemak serta Pesan Kesehatan untuk Pangan Olahan dan Pangan Siap Saji
Peraturan Menteri Kesehatan Republik Indonesia Nomor 41 tahun 2014 tentang Pedoman Gizi Seimbang
Permana, H., Nugraha, G. I., & Kariadi, S. H. K. S. (2012). Polimorfisme Gly972Arg Gen IRS-1 dan Cys981Tyr Gen PTPN1 sebagai Faktor Risiko pada Sindrom Metabolik dengan Riwayat Berat Bayi Lahir Rendah. Majalah Kedokteran Bandung. https://doi.org/10.15395/mkb.v44n3.137
Purnamasari, D. (2018). The Emergence of Non-communicable Disease in Indonesia. Acta Medica Indonesiana, 50(4).
Sanyaolu, A., Okorie, C., Marinkovic, A., Patidar, R., Younis, K., Desai, P., Hosein, Z., Padda, I., Mangat, J., & Altaf, M. (2020). Comorbidity and its Impact on Patients with COVID-19. SN Comprehensive Clinical Medicine. https://doi.org/10.1007/s42399-020-00363-4
Sigit, F. S., Tahapary, D. L., Trompet, S., Sartono, E., Willems Van Dijk, K., Rosendaal, F. R., & De Mutsert, R. (2020). The prevalence of metabolic syndrome and its association with body fat distribution in middle-aged individuals from Indonesia and the Netherlands: A cross-sectional analysis of two population-based studies. Diabetology and Metabolic Syndrome. https://doi.org/10.1186/s13098-019-0503-1
Sihombing, M., & Tjandrarini, D. H. (2015). Faktor Risiko Sindrom Metabolik pada Orang Dewasa di Kota Bogor. Penelitian Gizi Dan Makanan (The Journal of Nutrition and Food Research), 38(1), 21–30. https://doi.org/10.22435/pgm.v38i1.4418.21-30
Sitorus, C. E., Mayulu, N., & Wantania, J. (2020). Hubungan Konsumsi Fast Food, Makanan/Minuman Manis dan Aktifitas Fisik Dengan Kadar Gula Darah Dan Status Gizi Mahasiswa Fakultas Kedokteran Universitas Sam Ratulangi. Indonesian Journal of Public Health and Community Medicine, 1(4), 10-17.
Susilawati, S., Herdiani, I., & Novayanti, N. (2021). Gerakan Masyarakat Hidup Sehat (GERMAS) pada Kader Posyandu di Wilayah Puskesmas Cibeureum. Jurnal Abdimas PHB: Jurnal Pengabdian Masyarakat Progresif Humanis Brainstorming, 4(1), 41-46.
Tarawan, V. M., Fatimah, S. N., Nurhayati, T., Akbar, M. R., Radhiyanti, P. T., Purba, A., Akbar, I. B., & Goenawan, H. (2018). Association between metabolic syndrome criteria and lifestyle category among university academic staff in West Java, Indonesia. Pakistan Journal of Nutrition, 17(12), 709–714. https://doi.org/10.3923/pjn.2018.709.714
Zhu, S., St.-Onge, M. P., Heshka, S., & Heymsfield, S. B. (2004). Lifestyle behaviors associated with lower risk of having the metabolic syndrome. Metabolism: Clinical and Experimental, 53(11), 1503–1511. https://doi.org/10.1016/j.metabol.2004.04.017
Abraham, J. (2020, May 7). Manfaatkan Layanan Sehat Jiwa (SEJIWA): Tekan 119 ext. 8.
Psychology, BINUS University. https://psychology.binus.ac.id/2020/05/07/manfaatkan-layanan-sehat-jiwa-sejiwa-tekan-119-ext-8/
Arifuddin, Y. W. (2018, November 15). The Effect of Ruqyah Syar’iyyah Therapy on Anxiety,
Stress and Depression Among Health Science Students | Arifuddin | Holistic Nursing and Health Science. Holistic Nursing Health Science. https://ejournal2.undip.ac.id/index.php/hnhs/article/view/3417
Combating Mental Illness in Indonesia. (2019, May 25). BORGEN.
https://www.borgenmagazine.com/combating-mental-illness-in-indonesia/
Ermadi, P. S. (2018). Subjective USAbility Review of “Sehat Jiwa” Apps. Neliti.
https://www.neliti.com/publications/272218/subjective-usability-review-of-sehat-jiwa-apps
Hartini, N. (2018, October 31). Stigma toward people with mental health problems in Indonesia.
PubMed. https://pubmed.ncbi.nlm.nih.gov/30464658/
Ika. (2015). Minim Psikolog, Ribuan Penderita Gangguan Jiwa Belum Tertangani | Universitas
Gadjah Mada. Universitas Gadjah Mada. https://ugm.ac.id/id/berita/9715-minim-psikolog-ribuan-penderita-gangguan-jiwa-belum-tertangani
Indonesia Population (2020) - Worldometer. (2020). Worldometers.
https://www.worldometers.info/world-population/indonesia-population/
Mental Health Foundation. (2016, August 5). What is good mental health?
https://www.mentalhealth.org.uk/your-mental-health/about-mental-health/what-good-mental-health
More than one in four Indonesians experienced suicidal thoughts: Survey. (2019, June 23). The
Jakarta Post. https://www.thejakartapost.com/life/2019/06/23/more-than-one-in-four-indonesians-experienced-suicidal-thoughts-survey.html
National Center for Biotechnology Information. (2015, February 1). SUNDAR: mental health for
all by all. PubMed Central (PMC). https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5619600/
OECD. (2018). Promoting mental health in Europe: Why and how?
Kementerian Kesehatan RI. (2018, June 8). Pengertian Kesehatan Mental. Direktorat Promosi
Kesehatan Kementerian Kesehatan RI. https://promkes.kemkes.go.id/pengertian-kesehatan-mental
Prastiyani, A. (2019, July 26). Mental health care in Indonesia: short on supply, short on
demand. New Mandala. https://www.newmandala.org/mental-health-in-indonesia-short-on-supply-short-on-demand/
Sebayang, S. K., Mawarpury, M., & Rosemary, R. (2018, November 6). Less than 1,000
psychiatrists for 260 million Indonesians. The Jakarta Post. https://www.thejakartapost.com/academia/2018/11/06/less-than-1000-psychiatrists-for-260-million-indonesians.html
Singapore International Foundation. (2019, November 16). Mental health in Asia: The numbers.
Our Better World. https://www.ourbetterworld.org/series/mental-health/facts/mental-health-asia-numbers
State Government of Victoria. (2020, July 27). Promoting mental health and wellbeing in your
school. State Government of Victoria, Education and Training. https://www.education.vic.gov.au/school/teachers/health/mentalhealth/Pages/promoting-mental-health.aspx
U.S. Department of Health & Human Services. (n.d.). Talk About Mental Health For Educators.
https://www.mentalhealth.gov/talk/educators
Vikram Patel. (2012, September 11). Mental health for all by involving all [Video]. TED Talks.
https://www.ted.com/talks/vikram_patel_mental_health_for_all_by_involving_all
World Health Organization. (2019). MhGAP Community Toolkit: Mental Health Gap
Action Programme (mhGAP) (pp. 29-37, Rep.). World Health Organization. doi:10.2307/resrep27898.11
World Health Organization. (2020, July 2). Sustainable Development Goals.
https://www.who.int/health-topics/sustainable-development-goals
Aulia, N. (2020). Decade of Action for Road Safety dalam Meningkatkan Perilaku Pengguna Jalan Yang Berkeselamatan (Studi di Indonesia dan Thailand).
Badan Pusat Statistik. (n.d.). Retrieved January 23, 2021, from https://www.bps.go.id/publication/2020/11/20/ddce434c92536777bf07605d/statistik-transportasi-darat-2019.html
Guadamuz-Flores, R., & Aguero-Valverde, J. (2017). Bayesian Spatial Models of Crash Frequency at Highway–Railway Crossings. Transportation Research Record: Journal of the Transportation Research Board, 2608(1), 27–35. https://doi.org/10.3141/2608-04
Laporan Final LLAJ. (n.d.). Retrieved January 22, 2021, from http://knkt.go.id/post/read/laporan-final-llaj?cat=QmVyaXRhfHNlY3Rpb24tNjU
OECD iLibrary | Road safety. (n.d.). Retrieved January 22, 2021, from https://www.oecd-ilibrary.org/social-issues-migration-health/health-at-a-glance-asia-pacific-2020_65afc565-en
Organization, W. H. (2011). global launch. https://apps.who.int/iris/bitstream/handle/10665/82578/WHO_NMH_VIP11.08_eng.pdf
Road traffic injuries. (n.d.). Retrieved January 17, 2021, from https://www.who.int/news-room/fact-sheets/detail/road-traffic-injuries
Semarang), N. S. P. (Jurusan T. S. P. N. (2014). Mengenal Perilaku Pengendara Kendaraan Dalam Upaya Mencegah Terjadinya Kecelakaan Di Jalan Raya. Teknis, 9(1). https://doi.org/10.32497/TEKNIS.V9I1.685
Soehodho, S. (2017). Public transportation development and traffic accident prevention in Indonesia. In IATSS Research (Vol. 40, Issue 2, pp. 76–80). Elsevier B.V. https://doi.org/10.1016/j.iatssr.2016.05.001
Tingkat Kecelakaan Lalu Lintas Jalan di Indonesia Berdasarkan Data KNKT, S., & Dwi Saputra, A. (2007). Study of Traffic Accident Rate in Indonesia Base on KNKT (Komite Nasional Keselamatan Transportasi) Database from 2007-2016. Abadi Dwi Saputra Komite Nasional Keselamatan Transportasi (KNKT) Jl. Medan Merdeka Timur, 5, 10110. https://doi.org/10.25104/warlit.v29i2.557
WHO | Global status report on road safety. (n.d.). Retrieved January 17, 2021, from https://www.who.int/violence_injury_prevention/road_safety_status/report/en/
Agustina, R., Dartanto, T., Sitompul, R., Susiloretni, K. A., Achadi, E. L., Taher, A., ... & Khusun, H. (2019). Universal health coverage in Indonesia: concept, progress, and challenges. The Lancet, 393(10166), 75-102.
Bycroft, C., Freeman, C., Petkova, D., Band, G., Elliott, L. T.,Sharp, K., Motyer, A., Vukcevic, D., Delaneau, O.,O’Connell, J., et al. (2018). The uk biobank re-source with deep phenotyping and genomic data.Nature,562(7726), 203–209.
COVID-19 Host Genetics Initiative. (2020). The COVID-19 Host Genetics Initiative, a global initiative to elucidate the role of host genetic factors in susceptibility and severity of the SARS-CoV-2 virus pandemic. European Journal of Human Genetics, 28(6), 715.
Crossfield, S. S., & Clamp, S. E. (2013). Centralised elec-tronic health records research across health organ-isation types.International Joint Conference onBiomedical Engineering Systems and Technologies,394–406.
Cylus, J., Papanicolas, I., & Smith, P. C. (2017).How tomake sense of health system efficiency compar-isons?World Health Organization, Regional Officefor Europe Copenhagen.
Dartanto, T. (2014.). The study of optimal financial design of universal coverage of health insurance through CGE model analysis in the presence of informality in Indonesia: services, membership, premium, and willingness to pay. LPEM FEB-UI research report. Jakarta: Universitas Indonesia
Dartanto, T., Rezki, J. F., Siregar, C. H., Bintara, H., & Pramono, W. (2015). Expanding universal health coverage in the presence of informality in Indonesia: challenges and policy implications (No. 201511). LPEM, Faculty of Economics and Business, University of Indonesia.
Esteva, A., Kuprel, B., Novoa, R. A., Ko, J., Swetter, S. M.,Blau, H. M., & Thrun, S. (2017). Dermatologist-level classification of skin cancer with deep neuralnetworks.nature,542(7639), 115–118.
Gulshan, V., Peng, L., Coram, M., Stumpe, M. C., Wu, D.,Narayanaswamy, A., Venugopalan, S., Widner, K.,Madams, T., Cuadros, J., et al. (2016). Developmentand validation of a deep learning algorithm for de-tection of diabetic retinopathy in retinal fundus pho-tographs.Jama,316(22), 2402–2410.
Jiao, W., Atwal, G., Polak, P., Karlic, R., Cuppen, E., Danyi,A., De Ridder, J., van Herpen, C., Lolkema, M. P.,Steeghs, N., et al. (2020). A deep learning systemaccurately classifies primary and metastatic cancersusing passenger mutation patterns.Nature commu-nications,11(1), 1–12.
Kant, S., & Srivastava, M. M. (2018). Towards automatedtuberculosis detection using deep learning.2018IEEE Symposium Series on Computational Intelli-gence (SSCI), 1250–1253.
Lee, D., & Lee, J. (2020). Testing on the move: South Korea's rapid response to the COVID-19 pandemic. Transportation Research Interdisciplinary Perspectives, 5, 100111. https://doi.org/10.1016/j.trip.2020.100111
Mboi, N. (2015). Indonesia: On the way to universal healthcare.Health Systems&Reform,1(2), 91–97.
McGinnis, J. M., Olsen, L., Goolsby, W. A., Grossmann,C., et al. (2011).Clinical data as the basic stapleof health learning: Creating and protecting a pub-lic good: Workshop summary. National AcademiesPress.
Pham, T., Tran, T., Phung, D., & Venkatesh, S. (2017).Predicting healthcare trajectories from medicalrecords: A deep learning approach.Journal ofbiomedical informatics,69, 218–229.
Rajpurkar, P., Irvin, J., Zhu, K., Yang, B., Mehta, H., Duan,T., Ding, D., Bagul, A., Langlotz, C., Shpanskaya,K., et al. (2017). Chexnet: Radiologist-level pneu-monia detection on chest x-rays with deep learning.arXiv preprint arXiv:1711.05225.
Sirs yankes, url:http://sirs.yankes.kemkes.go.id/ [Accessed: 2020-01-20]
Social Security Agency for Health, 2018. Program management and financial report year 2014.2015.https://bpjs-kesehatan.go.id/bpjs/dmdocuments//49eff18ac9255bd6292dba43fa130fb3.pdf (accessed Oct 8, 2018).
Weintraub, W. S. (2019). Role of big data in cardiovascularresearch.Journal of the American Heart Associa-tion,8(14), e012791.
Zhang, L., Wang, H., Li, Q., Zhao, M.-H., & Zhan, Q.-M.(2018). Big data and medical research in china.bmj,360.
Agyemang, C., & van den Born, B.-J. (2018). Limited access to CVD medicines in low-income and middle-income countries: poverty is at the heart of the matter. The Lancet Global Health, 6(3), e234–e235. https://doi.org/10.1016/s2214-109x(18)30048-2
Bappenas/Kementerian PPN, Sekretariat Nasional SDGs. (2020, July 20). tujuan-3 |. http://sdgs.bappenas.go.id/tujuan-3/
Barizah, N. (2020). Indonesian Patent Policy on Compulsory License and Access to Affordable Medicines. European Journal of Molecular & Clinical Medicine, 7(5), 467-475.
Beck, E. J., Mandalia, S., DongmoNguimfack, B., Pinheiro, E., ‘t Hoen, E., Boulet, P., Stover, J., Gupta, A., Juneja, S., Habiyambere, V., Ghys, P., & Nunez, C. (2019). Does the political will exist to bring quality-assured and affordable drugs to low- and middle-income countries? Global Health Action, 12(1), 1586317. https://doi.org/10.1080/16549716.2019.1586317
BioFarma. (2020, March). Laporan Tahunan Bio Farma 2019. https://www.biofarma.co.id/
Bösenberg, S., & Egger, P. H. (2017). R&D tax incentives and the emergence and trade of ideas. Economic Policy, 32(89), 39–80. https://doi.org/10.1093/epolic/eiw017
BPPT. (2019, November 27). Tekan Impor Bahan Baku Obat, BPPT Gelar FGD Rencana Aksi Pengembangan Industri Parasetamol dan Amoksisilin. Https://Www.Bppt.Go.Id/. https://www.bppt.go.id/teknologi-agroindustri-dan-bioteknologi/3778-tekan-impor-bahan-baku-obat-bppt-gelar-fgd-rencana-aksi-pengembangan-industri-parasetamol-dan-amoksisilin
Chandna, H. (2020, February 26). What are APIs and how they threaten India’s status of a “pharmacy to the world.” ThePrint. https://theprint.in/theprint-essential/what-are-apis-and-how-they-threaten-indias-status-of-a-pharmacy-to-the-world/370941/
Carayannis, E. G., & Campbell, D. F. J. (2010). Triple Helix, Quadruple Helix and Quintuple Helix and How Do Knowledge, Innovation and the Environment Relate To Each Other? International Journal of Social Ecology and Sustainable Development, 1(1), 41–69. https://doi.org/10.4018/jsesd.2010010105
Clift, C., Gopinathan, U., Morel, C. M., Outterson, K., Røttingen, J. A., & So, A. (2015). Towards a new global business model for antibiotics: delinking revenues from sales. Chatham House.
Daryanto, C., & Daryanto, W. M. (2019). Financial Performance Analysis and Evaluation of Pharmaceutical Companies in Indonesia. International Journal of Innovation, Creativity and Change, 6(3), 207-224.
Hoen, E. (2015, February). Access to Cancer Treatment: A study of medicine pricing issues with recommendations for improving access to cancer medication (No. 978-1-78077-804–4). Oxfam International. http://hdl.handle.net/10546/344070
Herdady, M. R., & Muchtaridi, M. (2020). COVID-19: Alarm Bagi Sistem Rantai Pasok Industri Farmasi. Majalah Farmasetika, 5(4), 1. https://doi.org/10.24198/mfarmasetika.v5i4.27076
Hill, A. M., Barber, M. J., & Gotham, D. (2018). Estimated costs of production and potential prices for the WHO Essential Medicines List. BMJ Global Health, 3(1), e000571. https://doi.org/10.1136/bmjgh-2017-000571
Haider, N., Hollis, A., & Love, J. (2014). Delinkage proposals and the measurement of health benefits. Whittier Law Review, 38(3), 349-362.
Hidayat, T., & Darmawati, W. (2019). Reconstruction of Research Management in Indonesia. Journal of Science, Technology and Innovation Policy, 5(1), 6.
Hong, P., Kesselheim, A. S., & Sarpatwari, A. (2020). Transformative Models to Promote Prescription Drug Innovation and Access: A Landscape Analysis. Yale Journal of Health Policy, Law, and Ethics, 19(2), 2.
Irwanto, I. (2020). Comparative study of tax incentives in Indonesia, Malaysia, and the United States of America to support research and development (Doctoral dissertation, Universitas Pelita Harapan).
Kalbe. (2019). Annual Report 2019 KALBE. https://www.kalbe.co.id/investor/financial-reports-and-presentations/annual-report
Kementerian PPN/Bappenas. (2019, April). Kajian Sektor Kesehatan Penyediaan Obat, Vaksin Dan Alat Kesehatan (No. 978-623-93153-3–7). https://www.bappenas.go.id
Kasonde, L., Tordrup, D., Naheed, A., Zeng, W., Ahmed, S., & Babar, Z.-U.-D. (2019). Evaluating medicine prices, availability and affordability in Bangladesh using World Health Organisation and Health Action International methodology. BMC Health Services Research, 19(1), 1. https://doi.org/10.1186/s12913-019-4221-z
Kemenperin. (2020). Perkuat Struktur Industri Farmasi, Pemerintah Fasilitasi Insentif Investasi. https://kemenperin.go.id/artikel/20808/Perkuat-Struktur-Industri-Farmasi,-Pemerintah-Fasilitasi-Insentif-Investasi-
Kusumawardhani1, O.B., Ripha, R.W., (2020, December). Systematic Review: Kendali Mutu Dan Biaya Program Rujuk Balik (PRB) BPJS Kesehatan , PenguatanKolaborasi dan Kapasitas Perguruan Tinggi dalam riset dan pengabdian masyarakat di Era Pandemi Covid-19: Proceeding of University Research Colloqium 2020. ISSN:20479189
Kristina, S. A., Endarti, D., & Widayanti, A. W. (2020). PDG14 Evaluating Accessibility of Essential Medicines in Indonesia: A Survey on Availability and Price in Public and Private Health Sectors. Value in Health Regional Issues, 22, S40. https://doi.org/10.1016/j.vhri.2020.07.204
Ministry Of Science And Technology, Government of India. (2018, July). Drugs & Pharmaceutical Research. Https://Dst.Gov.in/Drugs-Pharmaceutical-Research.
Ministry of Commerce & Industry Department of Commerce Directorate General of Foreign Trade, Government of India. (2020, April 6). Amendment in Export Policy of APIs and formulations made from these APIs. http://89.187.84.168/FIEO/uploads/editor/fp/2jt4g4wn3qbn.pdf
National Institute of Pharmaceutical Education and research (NIPER). (2019). http://www.niperhyd.ac.in/about.html
OECD. (2021), Gross domestic spending on R&D (indicator). doi: 10.1787/d8b068b4-en
Ozawa, S., Shankar, R., Leopold, C., & Orubu, S. (2019). Access to medicines through health systems in low- and middle-income countries. Health Policy and Planning, 34(Supplement_3), iii1–iii3. https://doi.org/10.1093/heapol/czz119
Paulus, H., Erawan, I., & Mahaswari Jayanthi Mertha, A. (2020). Analisis Pengaruh Paket Kebijakan Ekonomi XVI terhadap Peningkatan Investasi di Indonesia Tahun 2019. E-Jurnal Politika, 1(2). Retrieved from https://ocs.unud.ac.id/index.php/politika/article/view/61969
Peraturan Pemerintah Nomor 9 Tahun 2016 tentang Perubahan atas Peraturan Pemerintah Nomor 18 Tahun 2015 tentang Fasilitas Pajak Penghasilan untuk Penanaman Modal di Bidang-bidang Usaha Tertentu dan/atau di Daerah-daerah Tertentu
Peraturan pemerintah Republik Indonesia Nomor 45 tahun 2019 tentang perubahan atas peraturan pemerintah nomor 94 tahun 2010 tentang perhitungan penghasilan kena pajak dan pelunasan pajak penghasilan dalam tahun berjalan
Samariadi. (2017). Pelaksanaan Compulsory Licensing Paten Obat-Obatan Bidang Farmasi Di Indonesia Dikaitkan Dengan Doha Declaration On The Trips Agreement And Public Health. Delegalata, 448. https://doi.org/10.31219/osf.io/jzq7b
Schuhmacher, A., Gassmann, O., & Hinder, M. (2016). Changing R&D models in research-based pharmaceutical companies. Journal of Translational Medicine, 14(1), 1. https://doi.org/10.1186/s12967-016-0838-4
Simanjuntak Rumondang. (2016). Pengawasan Bahan Baku Obat Untuk Mendukung Kemandirian Bahan Baku Obat. Badan Pengawasan Obat dan Makanan. [Slides]. https://Unpadwww.unpad.ac.id
Tarigan, I., & Suryati, T. (2018). Gambaran Out of Pocket pada Awal Era JKN di Indonesia. Jurnal Penelitian Dan Pengembangan Pelayanan Kesehatan, 141–146. https://doi.org/10.22435/jpppk.v1i2.536
Turcu-Stiolica, A., Subtirelu, M.-S., Taerel, A.-E., Boboia, A., & Berbecaru-Iovan, A. (2018). Analysis of Financial Losses due to Poor Adherence of Patients with Chronic Diseases and Their Impact on Health Economics. Financial Management from an Emerging Market Perspective, 1. https://doi.org/10.5772/intechopen.70320
UGM. (2018, February 22). UGM Kembangkan Vaksin Rotavirus Baru | Universitas Gadjah Mada. Ugm.Ac.Id. https://ugm.ac.id/id/berita/15749-ugm.kembangkan.vaksin.rotavirus.baru
Urias, E., & Ramani, S. V. (2020). Access to medicines after TRIPS: Is compulsory licensing an effective mechanism to lower drug prices? A review of the existing evidence. Journal of International Business Policy, 3(4), 367–384. https://doi.org/10.1057/s42214-020-00068-4
Urias, E. M. P. (2015). Improving access to HIV/AIDS treatment in Brazil: when are compulsory licenses effective in price negotiations?. Datawyse/Universitaire Pers Maastricht.
Vyas, N., Joshi, A., Malviya, S., & Kharia, A. (2020). Reduced Pharma Supply Chain in COVID-19: Measures to Reduce India’s Reliance for Active Pharmaceutical Ingredients on China and other Countries. Indian Journal of Pharmaceutical Education and Research, 54(4), 835–842. https://doi.org/10.5530/ijper.54.4.175
Wang, H., Sun, Q., Vitry, A., & Nguyen, T. A. (2017). Availability, Price, and Affordability of Selected Essential Medicines for Chronic Diseases in 11 Countries of the Asia Pacific Region: A Secondary Analysis. Asia Pacific Journal of Public Health, 29(4), 268–277. https://doi.org/10.1177/1010539517700472
Wartini, S. (2018). The Legal Implication of Compulsory Licence Pharmaceutical Products in the TRIPS Agreement to the Protection of the Right to Health in Developing Countries. Jurnal Dinamika Hukum, 18(1), 1-11.
Wesna, P. A. S. (2020). Doha Declaration sebagai Perlindungan Masyarakat atas Akses Obat Esensial di Negara Berkembang Pasca Trips Agreement. KERTHA WICAKSANA, 14(1), 56-62.
Downloads
Published
Categories
License

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.